Abstract
Background: Hodgkin Lymphoma (HL) and Non-Hodgkin Lymphomas (NHL) are hematologic neoplasms that require treatment with standard immune-chemotherapy and, in relapsed patients, intensification with hematopoietic stem cells transplantation (HSCT).
Introduction: Peripheral Inserted Central Venous Catheter (PICC) instead of a Peripheral Vascular Access and Centrally Inserted Central Venous Catheters (CICCs) could simplify HL and NHL patient management and allow a safer and effective therapy, according to their outpatient care.
Methods: Since its constitution in our Medical Oncology Department, a PICC team, consisting of a hematology physician and three dedicated nurses has carried out a prospective study to evaluate complication rate and usefulness of PICC device in the hematology clinical practice, particularly in HL and NHL patients. Inclusion criteria included all HL and NHL inpatient and outpatient who needed program of immune-chemotherapy, support treatment and HSCT, regardless of white blood cells (WBC) and platelets (PLT) counts. All patients underwent a previous evaluation of arms vascular anatomy by ultrasonography. All implantation procedures were performed under ultrasound guide with radiographic control following insertion.
Results: From March 2007 to June 2020, 316 PICC implantation were performed in 276 HL patients (156 males and 120 females) and 363 PICC in 322 NHL patients (178 males and 144 females). Median age for HL population was 36 years (range 16-85) and 58 (range 17-86) for NHL. In HL patients three hundred and five PICC (96,5%) were used for immune-chemotherapy courses, two (0,6%) for support treatment, seven (2,2%) for autologous HSCT, one (0,3%) for allogenic HSCT, one (0,3%) for tandem autologous-allogenic HSCT program. Similar data wad observed in NHL population: 333 PICC (91,7%) for immune-chemotherapy courses, 13 (3,6%) for support treatment, 14 (3,8%) for autologous HSCT, 3 (0,8%) for allogenic HSCT.
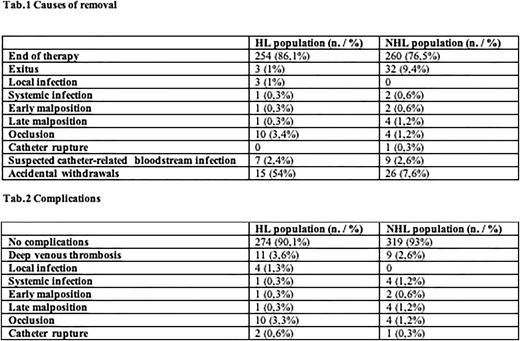
Twelve and twenty PICCs were lost at follow up respectively in HL and NHL population and for this reason the analysis about duration and complications was performed on 304 and 343 devices At the time of this analysis 9 out of 304 PICCs (2,9%) in HL patients and 3 out of 343 (0,9%) for NHL patients are still in situ and in use. The total duration of PICC-life was 50660 days (median 157; range 1 -828) for HL population and 43919 days (median 150; range 1-518) for NHL patients. The causes of removal in the two population are showed in Tab.1. Notably the most of PICCs in HL and NHL patients were removed for end of therapy (86,1% vs 76,5%) and none of suspected catheter-related bloodstream infection were confirmed through microbiological tests. The complication recorded in both populations are described in the Tab.2
More than 90% of PICCs did not show any kind of complications in both populations. Only 1 and 4 episodes of confirmed PICC-related septicemia (0.3%; 0,02/1000 days/PICC and 1,2%; 0,07/1000 days/PICC and) were recorded respectively in HL and NHL patients. The pathogens isolated in blood cultures and analysis of PICC tip were: Staphylococcus Epidermidis, Staphylococcus Hominis, Pseudomonas Aeruginosa and Candida Albicans. There were only 11 (3,6%; 0.25/1000 days/PICC) and 9 (2,6%; 0,17/1000 days/PICC) episodes of symptomatic PICC-related thrombotic complications in HL and NHL patients, without need of removal.
Conclusions. These data show that the use of PICC could be considered the device of choice in the management of HL and NHL patients because of easy insertion, safety of use, duration of life and low rate of complication, particularly in outpatient care.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal